As digital therapeutics become more
popular, it is important to consider how they can be integrated into mental
health care in an ethical manner. The path forward requires continued attention
both to appropriate oversight and models of care, and to issues of data
protection and justice.
Safety and Oversight Issues
The primary ethical concerns for digital
mental health technology have been safety, accountability, privacy, data
protection, transparency, consent, and bias and fairness (Table).1-3 Many consumer mental health apps are not regulated, and there have been related
concerns regarding the lack of evidence base for consumer mental health apps.4 Digital therapeutics are regulated as medical devices, and so the United States
Food and Drug Administration (FDA) provides oversight of safety and
effectiveness. However, formulating and implementing quality control measures
for algorithms used in digital therapeutics remains challenging, as does evaluating
the necessary external elements (ie, operating systems or connectivity) for
providing digital therapeutics. Many digital therapeutics are meant to evolve
continuously, which may mean that they need to be re-evaluated after an initial
certification.
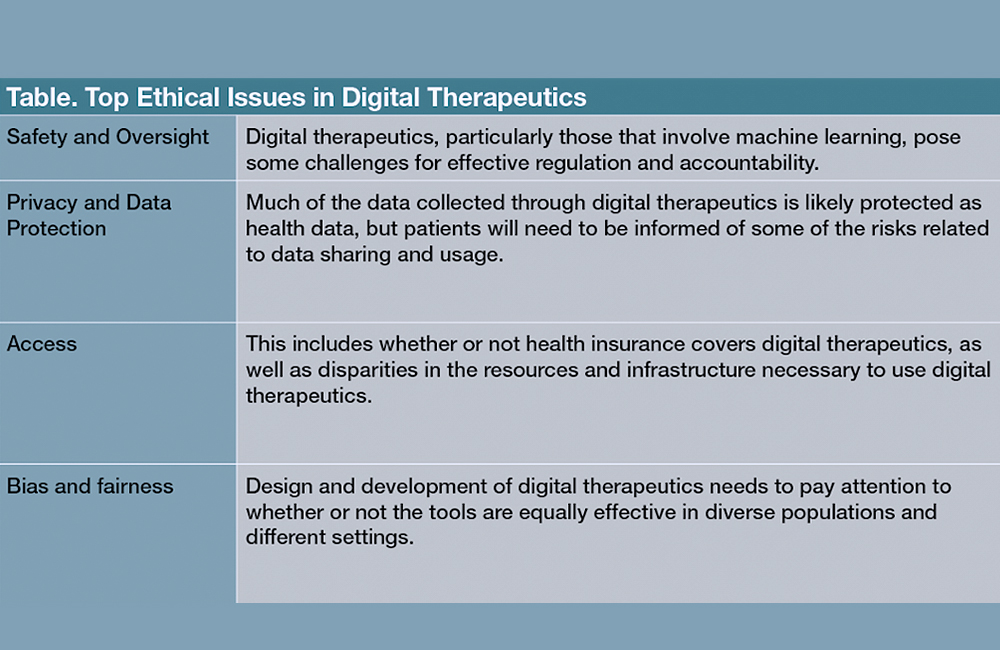
Table. Top Ethical Issues in Digital Therapeutics
The FDA’s Digital Software
Pre-Certification program certifies companies that are found to have “a robust
culture of quality and organizational excellence,” and then gives them a
streamlined process for product approvals.5 This program is meant to
address the challenges of regulating digital tools, but it has been criticized
for providing less stringent standards than those used for pharmaceuticals (eg,
lacking clarity regarding evaluation criteria and a complete definition of
excellence). Critics have also called for improved accountability for
maintaining standards.6 The regulation of medical devices in the
United States and Europe focuses on the product: the digital tool itself.
However, it is important to recognize that a digital tool will be used within
the context of a health delivery system, for purposes and goals specified
within that system, perhaps as part of a plan for allocating available
resources or for treating a particular patient population. Therefore, in order
to adequately assess the safety and efficacy of a digital tool, a systems view
regarding how that tool will be used is also necessary.7
Digital tools that rely on machine learning
present additional challenges for regulation. With machine learning algorithms,
it can be difficult to determine why specific data inputs led to a certain
output or findings.8 Consequently, it can be hard to evaluate and
address systematic problems in the outputs, such as biases that
disproportionately impact different populations.9,10 There are efforts to develop algorithms that are more explainable, but best
practices for identifying and addressing potential biases are still evolving.11 There have been calls for more transparency in health algorithms, such as
developers allowing for third-party review of algorithms. It is also important
for clinicians to carefully consider how to convey the risks and limitations of
digital therapeutic tools to patients for informed consent purposes. Clinicians
themselves may need training to understand the potential limitations of these
digital tools. Involving relevant stakeholders, from clinicians to patients and
community members, in plans for adoption and implementation of digital
therapeutics in a health care system, can also be helpful for addressing
fairness concerns.
Privacy and Data Protection
Mental health data are widely viewed as
more sensitive and potentially stigmatizing than other health data.12 Last year, a data security flaw in a popular psychotherapy app in Finland was
exploited by hackers, who then blackmailed thousands of users over their
personal data.13 This incident highlighted both the value of
behavioral information and the importance of strong data security measures. In
order to facilitate telehealth during the pandemic, the Office of Civil Rights
at the Department of Health and Human Services altered the Health Insurance
Portability and Accountability Act (HIPAA) Privacy Rule to eliminate penalties
for violations made in the good faith provision of telehealth.14 Although this provision and leniency is meant to end with the pandemic, there
will be continuing tension between the accessibility afforded by digital
technology, the potential exposure of patient data through these tools, and
appropriate balancing of accountability and liability concerns.
Data gathered through digital therapeutics
would generally be subject to HIPAA, which establishes protections for health
information used by covered entities (ie, health care providers, health plans,
and health care clearinghouses).15 The Health Information Technology
for Economical and Clinical Health Act further requires business associates of
a HIPAA-covered entity comply with the HIPAA Security Rule.16,17 There have been some incidents where business associates did not adequately
protect personal data.18 Digital therapeutics that are prescribed by
covered entities should have business associate agreements in place with the
digital therapeutic company and its associates that include provisions for
compliance.
Data brokerage is a $200 billion industry;
thus, the current landscape of data brokerage and sharing presents additional
concerns for the protection of patient data.19 Computer analytics
make it possible to draw behavioral health inferences from seemingly unrelated
information (ie, location data), and these inferences can lead to negative
ramifications for patients (ie, higher insurance rates or employment
discrimination).20-23 Although only de-identified data (data from
which 18 specific identifiers including name and age have been removed) may be
shared without restriction under HIPAA,24 advances in computing and
the availability of large public databases make re-identification of personal
data easier and more possible.25,26 Thus, de-identified patient data
that is shared with third-parties could be later re-identified and used in ways
that the patient may not have foreseen or expected.27 An increasing
number of jurisdictions have considered implementing personal and biometric
data regulations, such as the General Data Protection Regulation in the
European Union or the California Consumer Privacy Act.28 Against
this backdrop, clinicians’ patients need to appreciate the risks and benefits
regarding data collected through digital therapeutics; this information should
be conveyed through an informed consent process.
In addition, some digital therapeutics
continuously monitor patients, collecting a great amount of personal data.
Further studies should evaluate the impact of pervasive surveillance on
patients and the therapeutic alliance.
Bias and Fairness in Digital
Therapeutics
The COVID-19 pandemic, as well as the
recent social justice movements, have put a spotlight on bias and inequities in
the health care system.29,30 Due to historical injustices
experienced by Black and Latinx individuals in health care, these groups are
more likely to express concerns regarding privacy and the quality of digital
mental health.31
The shift to telehealth demonstrated that
not all communities or populations have the resources or infrastructure to take
advantage of digital tools. Community mental health centers, which
disproportionately serve Black and Latinx patients, are less likely to have the
necessary equipment.30 If digital therapeutics are to fulfill the promise of
increased access, improvements are needed in infrastructure, training, and
availability of clinician oversight to better serve low-income demographics.32 Associated resources, such as internet connection or hardware, may also be
needed.
Machine learning and digital health
technologies also raise issues of racial bias and fairness.33,34 There are different types of bias, such as an inadequate fit between the data
collected and the research purpose, datasets that do not have representative
samples of the target population, and digital tools that produce disparate
effects based on how they are implemented.35,36 If the research
population for creating the tools is not sufficiently representative of the
diverse contexts in which the digital therapeutics will be used, it can lead to
worse outcomes for certain groups or communities. There are a number of
approaches to addressing bias in digital health tools, such as technological
fixes in datasets and algorithms, or outlining principles for fairness in
algorithmic tools.
These are important measures, but there
must be a broader effort to detect the ways social inequities can shape the
development and efficacy of digital mental health tools.37 Although
digital therapeutics are regulated, it is important to note that the FDA has
not required data regarding diversity in training data for machine learning. In
a study of machine learning health care devices approved by the FDA,
investigators found that most of the 130 tools approved did not report if they
had been evaluated at more than 1 site, and only 17 provided demographic
subgroup evaluations in their submissions.38 Because the data
collected from some digital therapeutics may also be used for health research
purposes, digital tools that are of limited effectiveness or accessible to
select populations could exacerbate existing health care inequalities.
Developers, researchers, and clinicians
need to consider the usability and accessibility of digital therapeutics for
culturally diverse populations and marginalized groups.39 Digital
therapeutics should be evaluated on how well their designs and implementation
strategies take into account the needs of diverse populations (eg, individuals
from various age groups, races, gender, linguistic backgrounds, and disability
status). Engaging diverse stakeholders is vital for providing equitable mental
health care and avoiding a deeper digital divide in access. Future research
should inform best practices, particularly in terms of how digital therapeutics
interact with the provision of mental health services in real-world settings.
Concluding Thoughts
Telehealth and digital therapeutics hold
great promise in improving care for those with mental illness. It is, however,
important that we seek to integrate digital tools into mental health care in
ways that support, rather than disrupt, the therapeutic relationship and
provide equitable care.40-42
At the systems and policy levels, funding
and resources are needed to provide care for different mental health needs as
well as to broaden access to high-quality care for marginalized groups. Such
efforts will require attention to a range of issues, including reimbursement,
infrastructure, and developing appropriate care models (eg, stepped-care
models).43
Digital therapeutics raise questions about
appropriate lines of oversight or liability; they potentially impact the nature
of fiduciary relationships involved.44 Frameworks for how digital
therapeutics can address preventative care, patients in crisis, or special
populations (eg, those with severe mental illness) also need to be developed
and implemented. If we can meet these ethical challenges, then digital
therapeutics will provide not only innovative, but also equitable mental health
care.
Dr Martinez-Martin is assistant professor
at Stanford Center for Biomedical Ethics and in the Department of Pediatrics.
She has a secondary appointment in the Department of Psychiatry at Stanford
University’s School of Medicine. Safety and Oversight Issues
References
1. Martinez-Martin N, Dasgupta I, Carter A, et al.
Ethics of digital mental health during COVID-19: crisis and opportunities. JMIR
Ment Health. 2020;7(12):e23776.
2. Bauer M, Glenn T, Monteith S, et al. Ethical
perspectives on recommending digital technology for patients with mental
illness. Int J Bipolar Disord. 2017;5(1):6.
3. Torous J, Roberts LW. The ethical use of mobile
health technology in clinical psychiatry. J Nerv Ment Dis. 2017;205(1):4-8.
4. Weisel KK, Fuhrmann LM, Berking M, et al.
Standalone smartphone apps for mental health-a systematic review and
meta-analysis. NPJ Digit Med. 2019;2:118.
5. US Food and Drug Administration. Digital health
software precertification (pre-cert) program. September 11, 2020. Accessed
April 21, 2021.
https://www.fda.gov/medical-devices/digital-health-center-excellence/digital-health-software-precertification-pre-cert-program
6. Warren E, Murray P, Smith T. Letter to FDA on regulation
of software as medical device; 2018. October 10, 2018. Accessed July 6, 2021.
https://www.warren.senate.gov/oversight/letters/warren-murray-smith-press-fda-on-oversight-of-digital-health-devices
7. Gerke S, Babic B, Evgeniou T, Cohen IG. The need for
a system view to regulate artificial intelligence/machine learning-based
software as medical device. NPJ Digit Med. 2020;3:53.
8. Magrabi F, Ammenwerth E, McNair JB, et al.
Artificial intelligence in clinical decision support: challenges for evaluating
AI and practical implications. Yearb Med Inform. 2019;28(1):128-134.
9. Challen R, Denny J, Pitt M, et al. Artificial
intelligence, bias and clinical safety. BMJ Qual Saf. 2019;28(3):231-237.
10. Obermeyer Z, Powers B, Vogeli C, Mullainathan S.
Dissecting racial bias in an algorithm used to manage the health of
populations. Science. 2019;366(6464):447-453.
11. Amann J, Blasimme A, Vayena E, et al.
Explainability for artificial intelligence in healthcare: a multidisciplinary
perspective. BMC Med Inform Decis Mak. 2020;20(1):310.
12. Aitken M, de St Jorre J, Pagliari C, et al. Public
responses to the sharing and linkage of health data for research purposes: a
systematic review and thematic synthesis of qualitative studies. BMC Med
Ethics. 2016;17(1):73.
13. Ralston W. They told their therapists everything.
Hackers leaked it all. Wired. May 4, 2021. Accessed June 13, 2021.
https://www.wired.com/story/vastaamo-psychotherapy-patients-hack-data-breach
14. US Department of Health and Human Services.
Notification of enforcement discretion for telehealth remote communications
during the COVID-19 nationwide public health emergency. March 17, 2020.
Accessed April 24, 2020.
https://www.hhs.gov/hipaa/for-professionals/special-topics/emergency-preparedness/notification-enforcement-discretion-telehealth/index.html
15. Congress.gov. Health Insurance Portability and
Accountability Act of 1996. Public Law 104-191. August 21, 1996. Accessed July
15, 2021. https://www.congress.gov/104/plaws/publ191/PLAW-104publ191.pdf
16. US Department of Health and Human Services. HITECH
Act Enforcement Interim Final Rule. Reviewed June 16, 2017. Accessed July 15,
2021.
https://www.hhs.gov/hipaa/for-professionals/special-topics/hitech-act-enforcement-interim-final-rule/index.html
17. Perakslis ED. Cybersecurity in health care. N Engl
J Med. 2014;371(5):395-397.
18. Rothstein MA. Debate over patient privacy control
in electronic health records. Hastings Center, Bioethics Forum, 2011. Updated
February 5, 2014. Accessed July 6, 2021. https://papers.ssrn.com/sol3/papers.cfm?abstract_id=1764002
19. Crain M. The limits of transparency: data brokers
and commodification. New Media & Society. 2018;20(1):88-104.
20. Allen M. Health insurers are vacuuming up details
about you — and it could raise your rates. ProPublica. July 17, 2018. Accessed
July 6, 2021.
https://www.propublica.org/article/health-insurers-are-vacuuming-up-details-about-you-and-it-could-raise-your-rates
21. Wachter S. Data protection in the age of big data.
Nature Electronics. 2019;2(1):6-7.
22. Skiljic A. The status quo of health data
inferences. International Association of Privacy Professionals: Privacy
Perspectives. March 19, 2021. Accessed July 6, 2021.
https://iapp.org/news/a/the-status-quo-of-health-data-inferences/
23. Kröger JL, Raschke P, Bhuiyan TR. Privacy
implications of accelerometer data: a review of possible inferences. In:
Proceedings of the 3rd International Conference on Cryptography, Security and
Privacy. ICCSP ’19. Association for Computing Machinery; 2019:81-87.
24. De-identification of protected health information:
how to anonymize PHI. HIPAA Journal. October 18, 2017. Accessed July 6, 2021.
https://www.hipaajournal.com/de-identification-protected-health-information/
25. Benitez K, Malin B. Evaluating re-identification
risks with respect to the HIPAA privacy rule. J Am Med Inform Assoc.
2010;17(2):169-77.
26. Yoo JS, Thaler A, Sweeney L, Zang J. Risks to
patient privacy: a re-identification of patients in Maine and Vermont statewide
hospital data. Technology Science. October 9, 2018. Accessed July 6, 2021.
https://techscience.org/a/2018100901/
27. Culnane C, Rubinstein BIP, Teague V. Health data
in an open world. Cornell University. Computer Science. December 15, 2017.
Accessed July 6, 2021. http://arxiv.org/abs/1712.05627
28. California Consumer Privacy Act of 2018
[1798.100-1798.199.100]. California Legislative Information. Updated November
3, 2020. Accessed July 15, 2021.
https://leginfo.legislature.ca.gov/faces/codes_displayText.xhtml?division=3.&part=4.&lawCode=CIV&title=1.81.5
29. Webb Hooper M, Nápoles AM, Pérez-Stable EJ.
COVID-19 and racial/ethnic disparities. JAMA. 2020;323(24):2466-2467.
30. van Deursen AJ. Digital inequality during a
pandemic: quantitative study of differences in COVID-19-related internet uses
and outcomes among the general population. J Med Internet Res.
2020;22(8):e20073.
31. George S, Hamilton A, Baker RS. How do low-income
urban African Americans and Latinos feel about telemedicine? A diffusion of
innovation analysis. Int J Telemed Appl. 2012;2012:715194.
32. Conrad R, Rayala H, Diamond R, et al. Expanding
telemental health in response to the COVID-19 pandemic. Psychiatric Times.
April 7, 2020. Accessed July 6, 2021.
https://www.psychiatrictimes.com/view/expanding-telemental-health-response-covid-19-pandemic
33. Rajkomar A, Hardt M, Howell MD, et al. Ensuring
fairness in machine learning to advance health equity. Ann Intern Med.
2018;169(12):866-872.
34. Gerke S, Minssen T, Cohen G. Ethical and legal
challenges of artificial intelligence-driven healthcare. In: Bohr A, Memarzadeh
K, eds. Artificial Intelligence in Healthcare. Elsevier;2020:295-336.
35. Char DS, Shah NH, Magnus D. Implementing machine
learning in health care-addressing ethical challenges. N Engl J Med.
2018;378(11):981-983.
36. Binns R. Fairness in machine learning: lessons
from political philosophy. Cornell University. Computer Science. Updated March
23, 2021. Accessed July 6, 2021. http://arxiv.org/abs/1712.03586.
37. Mittelstadt B. Principles alone cannot guarantee
ethical AI. Nat Mach Intell. 2019;1(11):501-507.
38. Wu E, Wu K, Daneshjou R, et al. How medical AI
devices are evaluated: limitations and recommendations from an analysis of FDA
approvals. Nat Med. 2021;27(4):582-584.
39. Martschenko D, Martinez-Martin N. What about
ethics in design bioethics? Am J Bioeth. 2021;21(6):61-63.
40. Martinez-Martin N, Dunn LB, Roberts LW. Is it
ethical to use prognostic estimates from machine learning to treat psychosis?
AMA J Ethics. 2018;20(9):E804-811.
41. Potier R. The digital phenotyping project: a
psychoanalytical and network theory perspective. Front Psychol. 2020;11:1218.
42. Dagum P, Montag C. Ethical considerations of
digital phenotyping from the perspective of a healthcare practitioner. In:
Baumeister H, Montag C, eds. Digital Phenotyping and Mobile Sensing: New
Developments in Psychoinformatics. Springer International Publishing;
2019:13-28.
43. Taylor CB, Fitzsimmons-Craft EE, Graham AK.
Digital technology can revolutionize mental health services delivery: the
COVID-19 crisis as a catalyst for change. Int J Eat Disord.
2020;53(7):1155-1157.
44. Cohen IG, Amarasingham R, Shah A, et al. The legal
and ethical concerns that arise from using complex predictive analytics in
health care. Health Aff (Millwood). 2014;33(7):1139-1147.